PORTLAND, Maine — Dr. Andrea Nazarenko is a psychologist, and author of When Food Hurts: 4 Steps to a Gut-Happy Lifestyle. She talks about the importance of healthy, clean eating, and why that plays a factor in not only physical health, but mental health.
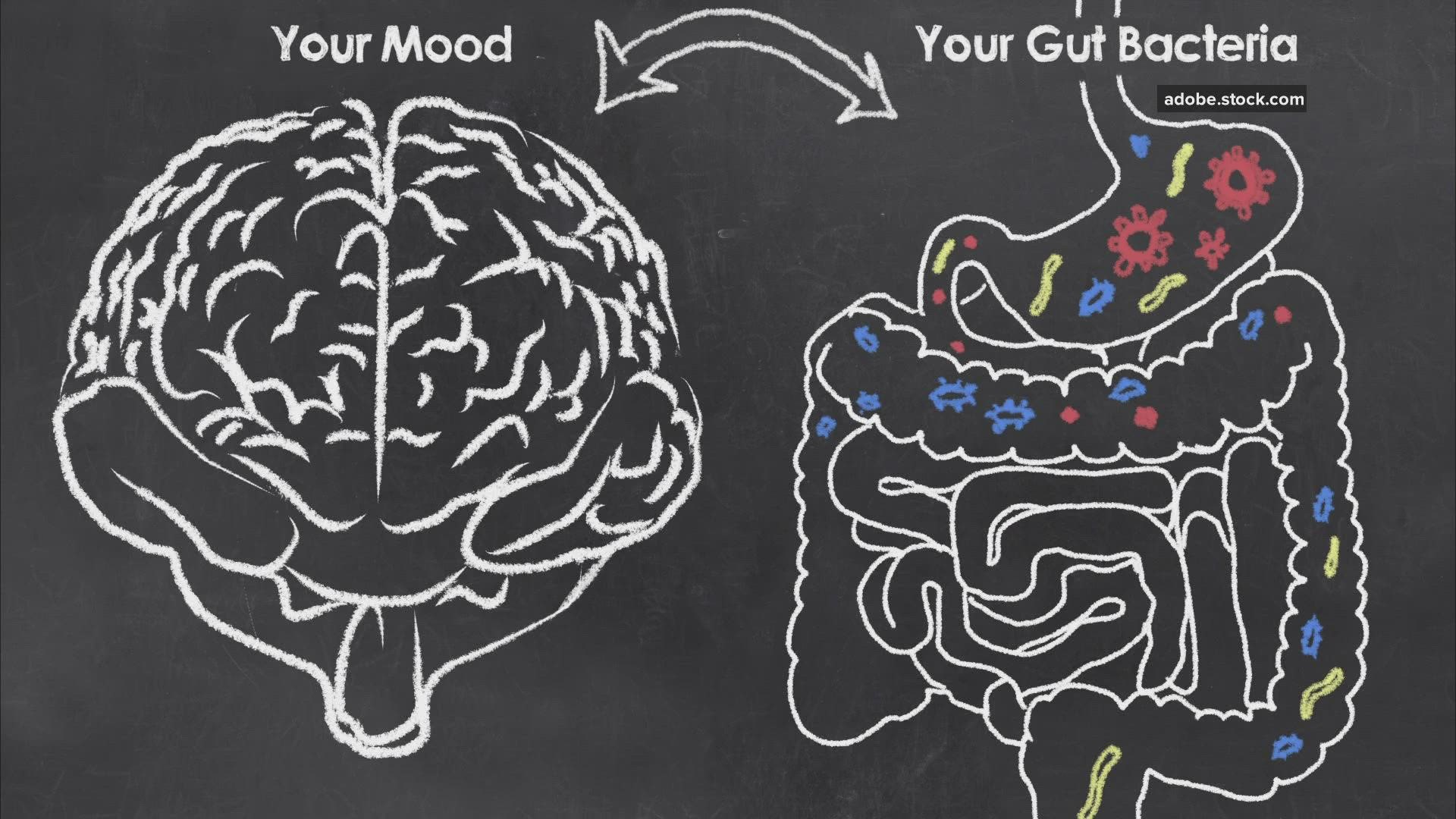
Just as our heart and lungs cannot function optimally without proper nutrition, our brain cannot function optimally without fueling it with the nutrition it needs. This means that what we eat determines how we feel… and the answer to unlocking your anxiety or depression may not be in your brain, but rather your GUT!
The “Feel Good” Bugs & Our Second Brain
To understand the complex ways that food impacts our mood, we have to look beyond our plate and to a magnificent world of microscopic organisms living inside of us. Termed the microbiome, this ecosystem filled with microscopic creatures plays a critical – yet often overlooked – role in shaping our emotional, mental, and physical health.
The gut-brain axis refers to the direct and indirect communication between the gut and the brain. This pathway plays a huge role in our stress response and mental health. Science demonstrates the importance of the gut in a growing number of psychiatric, neurodevelopmental, age-related, and neurodegenerative disorders, including autism spectrum disorders, anxiety, depression, bipolar disorder, schizophrenia, Parkinson’s disease, and Alzheimer’s disease.
A Healthy Gut Is a Key to a Healthy Brain
The trillions of microorganisms that live in our gut play a huge role in how the brain functions. An unhealthy gut may lead to imbalances in neurotransmitters, neuroinflammation, and may even alter the way that your body perceives and handles stress. This can lead to mood disorders such as depression or anxiety which are considered chemical imbalances in the brain. If neurochemical imbalances identified in the brain are the result of an imbalance in the gut, it follows that we can balance the gut to balance the mind. Early work on both probiotic and dietary interventions shows high efficacy and promise for effective treatments in the future.
Stress and Mood
There is no doubt that stress and mood are like closely related cousins. Both chronic and acute stress contribute to the onset and severity of mood problems like anxiety and depression. Still, there are major differences in the ways people handle stress, leading psychologists to wonder “why”? While some people feel overwhelmed and suffer a negative mood under conditions of stress, others demonstrate resilience. One newly discovered reason is the health of the microbiome. Microbiomes that contain a diverse, stable, and resilient ecosystem support the host’s (person’s) ability to handle stress. When an individual has an unhealthy gut, they are more susceptible to the effects of stress. A person with an unhealthy gut may perceive the same environment as more stressful than a person with a healthy gut.
A Gut-Happy Lifestyle
A “Gut Happy Lifestyle” involves adding the good and removing the bad. You can start by adding the good and removing the bad on your plate. The Standard American Diet (SAD) is a common dietary pattern in the United States characterized by a high intake of ultra-processed foods, foods with added sugar, high-fat, and high sodium; and minimal fruits, vegetables, whole grains, legumes, and lean protein. This type of diet supports an unhealthy gut. Eating a diet diverse in plants, healthy fats, and nutrients feeds the “good guys,” supporting a healthy microbiome and overall physical, mental, and emotional health.
A healthy diet is only part of the formula for health. It’s also important to consider how you eat and live. In traditional Mediterranean countries, the culture around eating differs from that of the modern American meal. Instead of rushing from meal to meal, shoving foods down your throat before the next “to do” item on your list, make mealtime special. Schedule time to eat with people you love and be mindful of your eating practices. Share stories and create memories over a meal. Health is mind, body, and soul. Mealtime can be an opportunity to support all three of these dimensions.
Lifestyle choices — such as diet, toxin exposure, infections, use of antibiotic medications, environmental stressors, alcohol, OTC and prescription drugs (including NSAIDS), and emotional stress — all contribute to gut health, too.
The Mediterranean Diet
One of the best diets for gut health is known as the Mediterranean Diet. This diet is based on the traditional dietary habits of people living in countries bordering the Mediterranean Sea, such as Italy, Greece, and Spain. It is based on a set of dietary principles and lifestyles, rather than lists of “approved foods” that one can eat on the diet.
The foundation of a Mediterranean-style diet includes an abundance of plants (fruits, vegetables, whole grains, nuts, and legumes) that are minimally processed, pesticide-free, consumed in season, and locally grown. The diet supports the daily intake of olive oil, as a primary source of fat. Cheese and yogurts are also recommended daily, consumed in low to moderate amounts. In terms of animal meats, fish and poultry are recommended a few times a week in low to moderate amounts; and red meats are recommended infrequently in small portions. Wine is permitted in moderation, recommended at meals. Water should be the primary liquid intake.
Foods that should be avoided include any foods with added sugar, sweets (fruit can be eaten as desserts and raw honey as a sweetener in moderation), sweetened beverages (including sodas, energy drinks, sweet tea, and other sweetened drinks), refined grains, trans fats, refined oils, processed meat, and highly processed foods (including anything labeled “low-fat” or “diet” or looks like it was made in a factory).
While not part of the Mediterranean Diet, I also suggest removing gluten to support gut and mental health.
At a glance, a Mediterranean-style diet follows the following guidelines:
Daily: Fruit, vegetables, whole grains (choose gluten-free for gut health), extra virgin olive oil, beans, nuts, legumes, seeds, herbs, and spices.
Moderation: Fish & Seafood (choose sustainable and low mercury), poultry, eggs, cheese, & yogurt.
Rarely: Red Meat.
Drink: Mostly water. If you drink alcohol, enjoy wine in moderation.
As a general rule of thumb, if the food came from the Earth and was living at some point, consider eating it. If it was made in a factory or has long lists of ingredients that you do not recognize, consider avoiding it.
Is Eating Well All It Takes?
The science is accumulating that demonstrates the connection between the mind and the gut. This cutting-edge information, however, does not replace what we know about mental illness. Chronic stress from current or past traumas also plays a role. Toxic thoughts, past traumas, and/or ongoing stress contribute directly and indirectly to problems with mood. If you are suffering from mental illness, consider dietary changes as an adjunct alongside traditional, evidence-based talk therapies to address both cognitive and physical aspects of mood. While it is known that a healthy diet supports mental and physical health, the research on diet in the onset and treatment of diagnosable mental illness remains inconclusive.